Scientists are hopeful that Paxlovid may help guard against long COVID : Shots

Patients had a prolonged reduced risk of developing COVID after taking Paxlovid, and benefits were seen in vaccinated and unvaccinated individuals.
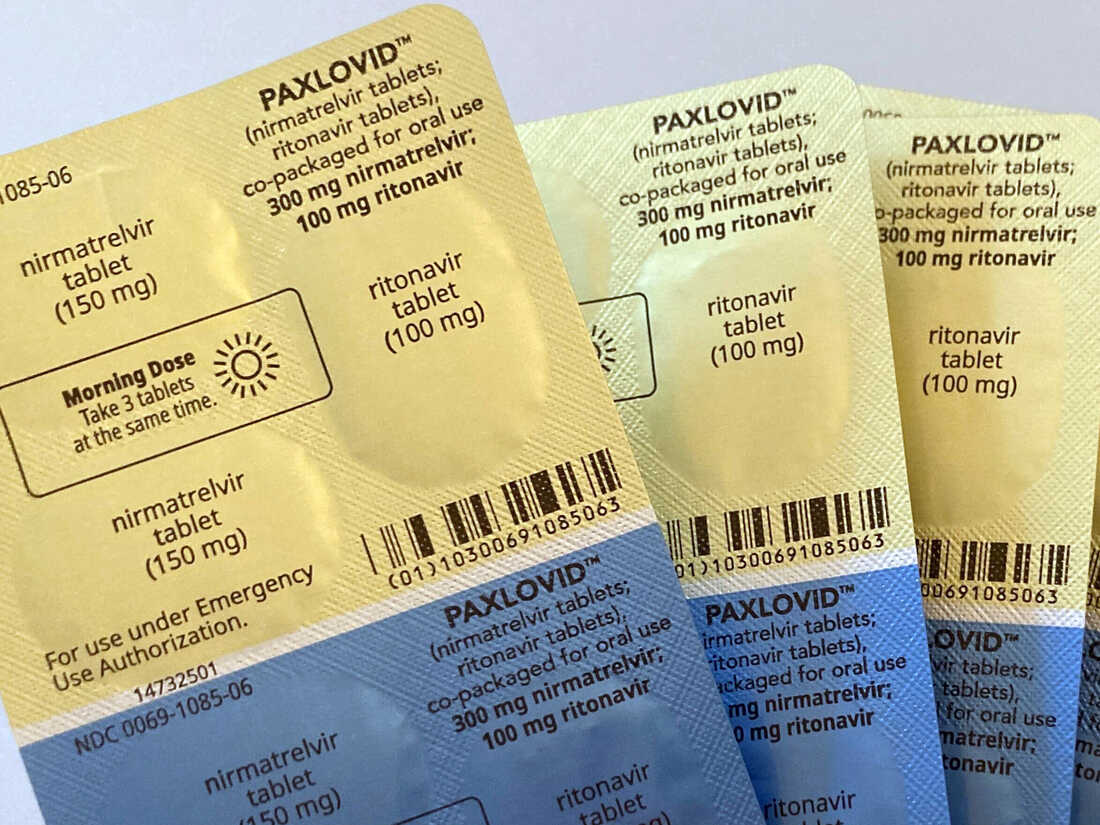
Stephanie Nano / AP
hide captions
switch captions
Stephanie Nano / AP

Patients had a prolonged reduced risk of developing COVID after taking Paxlovid, and benefits were seen in vaccinated and unvaccinated individuals.
Stephanie Nano / AP
There is extensive literature that Paxlovid – a 5-day antiviral drug from Pfizer – can reduce the risk of hospitalization in COVID-19 patients, who are more likely to develop severe illness.
Now, researchers from the Veterans Affairs Health Administration have found that taking the drug may also reduce the risk of developing long-term COVID, according to a new study. new research was posted online this weekend and has not yet undergone peer review.
“We’ve known for a long time that Paxlovid reduces the risk of acute problems,” Dr. Ziyad Al-AlyLead research and development team at VA Saint Louis Healthcare System, and study co-author, “We are now adding to the observation that Paxlovid also reduces the risk of persistent COVID. “
This drug, which has been available in the US for nearly a year, is provided free of charge by the federal government in pharmacies nationwide. It requires a prescription and patients with COVID-19 must start it within five days of symptom onset.
Less virus, less COVID longer?
In the study, persistent COVID was defined as developing one or more symptoms – including heart problems, blood disorders, fatigue and shortness of breath – one to three months after testing positive. According to these figures, patients taking Paxlovid were 26% less likely to have persistent COVID.
To reach this finding, the researchers looked at electronic health records from more than 56,000 patients in the VA health system who tested positive for COVID-19 between March and June 2022. and have at least a risk factor for serious illness. They compared the health outcomes of 9,000 patients who had taken Paxlovid early in their illness, with 47,000 patients who did not.
The benefits of taking Paxlovid don’t just apply to people who have not been vaccinated. Patients who had been vaccinated or boosted, or had repeated COVID-19 infections, had a similar reduction in their risk of developing long-term COVID, the study found.
The study is a preprint, which means it was shared publicly before being reviewed and edited by external researchers. But experts not involved in the study told NPR that the findings make sense, given how Paxlovid works.
Antiviral drugs prevent viruses from multiplying in cells. “We know that one of the key factors in predicting the persistence of COVID is that the virus is detectable in the blood at the time of infection.” Dr. Peter Chin-Hong, an infectious disease physician at the University of California, San Francisco, wrote in an email. “So it makes sense that interventions that prevent the virus from making more copies of itself would lead to a lower risk of long-term COVID.”
Previous studies have shown that Paxlovid reduces the risk of hospitalization and death from COVID-19. “Since the causative agent of long-term COVID is acute infection with SARS-CoV-2, it feels intuitive that anything that reduces the severity of this infection will reduce the risk of long-term COVID,” whether it’s Paxlovid or other antiviral treatments,” Dr. Paul Saxan infectious disease physician at Brigham and Women’s Hospital in Boston, wrote in an email.
A starting point
However, experts see this study as just a starting point to explore the potential uses of Paxlovid. The VA study is observational, based on data entered into the patient’s health records – in Sax’s view, “the inaccuracies of [long COVID] Making a definitive diagnosis from this study is challenging, especially with a retrospective review. ”
But the value of the study is that it shows researchers promising avenues for further research, Dr. Monica Gandhi, an infectious disease physician at UCSF. “It’s hypothetical,” she said, “It’s exciting and hopeful [to think] that if you reduce the viral load… to undetectable levels [early in the illness]maybe you can prevent post-COVID symptoms altogether” — a theory she thinks researchers could pursue.
Both Sax and Gandhi said they would feel more confident in the results if they were replicated in additional studies, especially in randomized controlled trial comparing sustained COVID outcomes in patients receiving Paxlovid or placebo. The findings of the VA study were also limited by the fact that the participants were predominantly white men, raising the possibility that the benefits of Paxlovid may differ in other patient populations.
Currently, Paxlovid only allowed to use in patients with risk factors – such as being older or having underlying health conditions – that put them at high risk of developing severe disease. Al-Aly said the sustained reduction in COVID risk, outlined in his study, suggests that others may also benefit from taking Paxlovid. But many patients with long-term COVID-19 were relatively young and healthy before they got COVID-19 and may not be eligible for Paxlovid when they test positive, he said.
“Does the use of Paxlovid reduce the risk of acute problems and subsequently the risk of persistent COVID?” Al-Aly wondered, “I think that’s a question we all need to address over the next few months.”
It is also an open question whether a higher dose or a longer course of treatment might provide greater benefit, Chin-Hong said.
Side Effects including nausea and discomfort caused the patient to pause using the product. Reports of COVID recovery in Paxlovid patients, where the illness flared up after a seemingly respite, have led some prescribers to have mixed opinions about the product. Al-Aly says these are real considerations, but they should be weighed against the benefits of Paxlovid treatment, including reduced risk of hospitalization and death in the acute phase, and potential avoidance of COVID. continued in the following months.
Gandhi said the study’s findings could now influence clinicians’ decisions, even if the results are preliminary and have not been replicated.
“This research is motivating me to use [Paxlovid] in people over 65, vaccinations and boosters are recommended, because it will likely have benefits other than preventing hospitalization,” she said.




